Mycoplasma: The Chronically-Overlooked Infection
What is Mycoplasma?
Mycoplasma is the smallest free-living and self-replicating species of bacteria that infects the human body. The mycoplasma cell contains the minimum set of organelles essential for growth and replication: a plasma membrane, ribosomes, and a genome consisting of a double-stranded circular DNA molecule. Unlike all other prokaryotes, the mycoplasmas have no cell walls, and they are consequently placed in a separate class Mollicutes (mollis, soft; cutis, skin).
Mycoplasma is highly pleomorphic, meaning that it does not have a fixed shape. This quality enables it to alter its shape and size for survival and to cross filters that are otherwise only permeable to viruses, making this infection difficult to detect if it is chronic. Mycoplasmas have been nicknamed the “crabgrass” of cell cultures because their infections are persistent, frequently difficult to detect and diagnose, and difficult to cure. However, acute infections are rather easy to diagnose through lab testing.
Mycoplasma is commonly known for causing acute “walking pneumonia” and various respiratory illnesses. The specific strain that causes these ailments is known as Mycoplasma pneumoniae. This infection occurs worldwide and is more prevalent in colder months. It affects mainly children ages 5 to 9 years. Additionally, it is spread by close personal contact and has a long incubation period.
However, acute infections such as “walking pneumonia” are just one type of infection that may occur from exposure to mycoplasma. In fact, chronic mycoplasma infections are seen throughout multiple chronic illnesses and are transmitted by other routes.
Symptoms of a Chronic Mycoplasma Infection:
Symptoms of a chronic mycoplasma infection differ from acute infections such as “walking pneumonia.” Not all symptoms need to be present in order to be affected by a mycoplasma infection. Symptoms include:
Sinus Congestion
Dry Cough
Rashes / Skin Issues
Chronic Fatigue / Easily Tired
Fever
Frequent Headaches
Lung Issues (Recurring Bronchitis/Pneumonia, Fluid Accumulation)
Muscle / Joint Pain
Sore Throat
Wheezing
What is a Chronic Mycoplasma Infection?
Chronic mycoplasma infections may be caused by human-to-human contact, food contamination, or via tick bite. Since mycoplasma is also a Lyme co-infection, it can affect those with Lyme disease.
The immune system recognizes mycoplasma as a secondary threat as it prioritizes the microbes or toxins that are currently perceived to be most dangerous to the body. Typically these microbes or toxins include: Lyme disease, Lyme co-infections, mold exposure, parasites, heavy metals, environmental toxins, gastrointestinal dysbiosis, viruses, etc. Due to this, mycoplasma is an opportunistic infection, meaning that it affects the body when it is suppressed by microbes or toxins. Oftentimes, mycoplasma will make itself known when paired with those primary threats.
How Does Mycoplasma Affect People With Lyme Disease?
According to a 2019 study, mycoplasma infects 82% of people with Lyme disease. Additionally, there has been a 320% increase in the number of US counties affected within the past 20 years. In otherwise healthy people, mycoplasma will only cause mild and/or acute symptoms. However, if a person is infected with mycoplasma in addition to Lyme disease, symptoms may be severe. It is evident that these two infections compliment each other in debilitating ways, leading to exacerbated symptoms that may be seen as “random.” The most predominant strains of mycoplasma in Lyme patients are M. fermentans and M. pneuomniae.
A 2012 study states that “the differential diagnosis between Lyme disease and Mycoplasma pneumoniae infection or the recognition of the co-infection by Mycoplasma pneumoniae is problematical because both diseases exhibit similar manifestations; this applies to the extrapulmonary manifestations of Mycoplasma pneumoniae infection: disorders of the CNS, musculoskeletal system, heart, kidney and eye.”
Another 2007 study found that “68.75% of Chronic Fatigue Syndrome (CFS)/Lyme patients show evidence of mycoplasma coinfections.” The U.S. Department of Health and Human Services states that “the fact that patients with Lyme disease have this systemic infection [mycoplasma] at much higher rates than many other common Lyme bacterial and viral co-infections suggests that this is an important co-infection in Lyme patients.”
Additionally, people with a mycoplasma infection are more susceptible to rheumatoid arthritis (RA). Arthritis and joint pain are two common symptoms of Lyme disease and are often caused or exacerbated by a Lyme-coinfection such as mycoplasma.
Although mycoplasma is typically seen as a not-so-dangerous Lyme co-infection in comparison to babesia, bartonella, rickettsia, ehrlichia, etc., but it may cause severe damage if it is the most prevalent infection in the body. If the body heals from a complimentary Lyme co-infection, but does not heal from the lingering mycoplasma infection, additional symptoms may arise.
Click here to read our article on Lyme disease and Lyme co-infections!
Can Mycoplasma Contribute to Other Chronic Illnesses or Symptoms?
Yes - absolutely. Since mycoplasma does not have a cell wall, its shape shifts and alters its size, making it difficult to detect. Since the organism is so small, it may infect any part of the body and interact with a variety of infections and toxicities.
Conditions, infections, and toxicities that mycoplasma contribute to are:
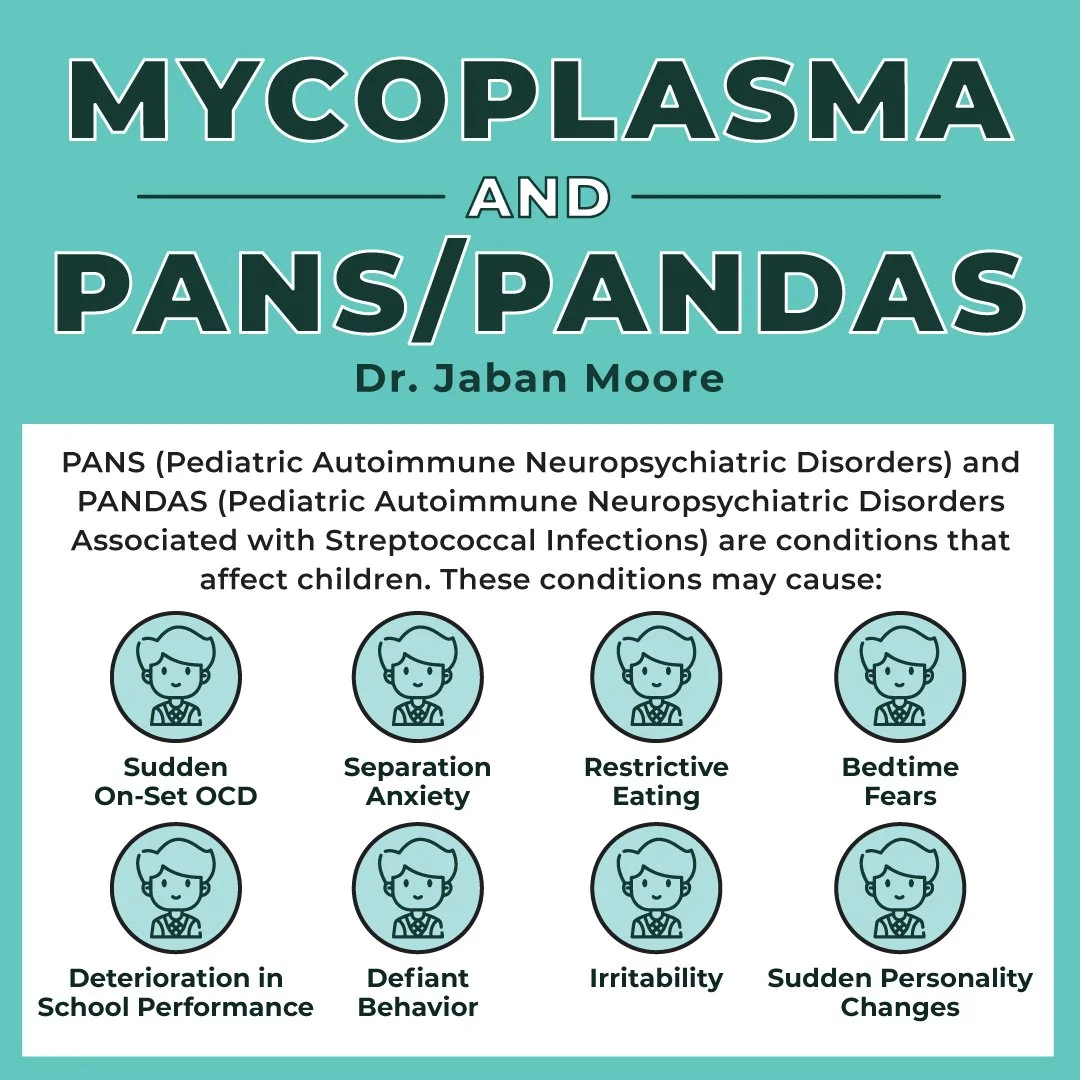
1) PANS/PANDAS: Mycoplasma, specifically M. pneumoniae infections, are common in children, and they can be present as an important co-infection with other bacteria and toxins. PANS/PANDAS affects the basal ganglia, the brain structure responsible for motor control, as well as motor learning, executive functions and behaviors, and emotions.
According to a 2014 study “neurological manifestations associated with M. pneumoniae infections usually resolve completely, but they can result in chronic debilitating deficits in motor or mental function with varying degrees.” Mycoplasma has been proven to cause abnormal signals in the basal ganglia.
Additionally, it is seen that neurological symptoms occur in 25% of hospitalized pediatric patients with M. pneumoniae infection.
Click here to read our article on PANS/PANDAS!
2) Mold Toxicities: Mycoplasma symptoms and mold toxicity symptoms often overlap. However, when mycoplasma and mold are paired together, they may cause massive cytokine storms. This is a severe immune reaction in which the body releases too many cytokines into the blood too quickly. Cytokines play an important role in normal immune responses, but having a large amount of them released in the body all at once can be harmful.
If there is an ongoing cytokine storm, pro-inflammatory cytokines will cause systemic inflammation and symptoms of whatever infection or toxicity the body is actively dealing with.
Click here to read our article on mold toxicities!
3) Speech and Developmental Disorders: According to a 2017 study, “manifestations of Mycoplasma pneumoniae infection can range from self-limiting upper respiratory symptoms to various neurological complications, including speech and language impairment.” The study showed that a “Mycoplasma pneumoniae infection was significantly associated with greater incidence of speech and language impairment [hazard ratio (HR) = 1.49, 95% CI: 1.23–1.80].”
Another 2007 study found that “a large subset (28/48 or 58.3%) of [autism spectrum disorder (ASD)] patients showed evidence of Mycoplasma spp. infections compared with two of 45 (4.7%) age-matched control subjects (odds ratio = 13.8, P < 0.001).”
Mycoplasma is commonly found in children with developmental or neurological disorders.
4) Tourette’s Syndrome: Tourette’s Syndrome (TS) is a the most common tic disorder and is characterized by motor and vocal or phonic tics typically beginning in childhood, often accompanied by obsessive–compulsive disorders, poor impulse control and other behavioral problems.
According to a 2004 study, “elevated titers [of Mycoplasma pneumoniae] were found in significantly more TS patients than controls (17 vs. 1). Additionally, the number of IgA positive patients was significantly higher in the TS group than in the control group (9 vs. 1). A higher proportion of increased serum titers and especially of IgA antibodies suggests a role for M. pneumoniae in a subgroup of patients with TS and supports the finding of case reports implicating an acute or chronic infection with M. pneumoniae as one etiological agent for tics.”
How Can I Test for Mycoplasma?
Unfortunately, chronic mycoplasma infections are difficult to test for as it is the smallest species of bacteria. However, antibody testing or PCR testing is the most reliable. Vibrant Labs and Igenex also offer Lyme disease and Lyme co-infection testing that test for certain strains of mycoplasma.
If you believe you are dealing with chronic illness, please contact a functional provider. Dr. Jaban Moore, a functional medicine provider, can help you if you are experiencing chronic symptoms.
Please reach out if you are interested in taking your health back! You can give our office a call at (816) 889-9801.
References:
https://pubmed.ncbi.nlm.nih.gov/15590039/
https://www.sciencedirect.com/topics/medicine-and-dentistry/gilles-de-la-tourette-syndrome
https://pubmed.ncbi.nlm.nih.gov/17265454/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5495436/
https://erj.ersjournals.com/content/37/6/1431
https://www.cancer.gov/publications/dictionaries/cancer-terms/def/cytokine-storm
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4444319/
https://www.thieme-connect.de/products/ejournals/abstract/10.1055/s-0036-1584325
https://pubmed.ncbi.nlm.nih.gov/22244792/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4359422/ https://pubmed.ncbi.nlm.nih.gov/28538981/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6401534/
https://pubmed.ncbi.nlm.nih.gov/15590039/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6331094/
https://www.hhs.gov/ash/advisory-committees/tickbornedisease/reports/other-tbds-2018-5-9/index.html
https://www.tandfonline.com/doi/abs/10.3109/10573320802091809
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3565243/
https://www.ncbi.nlm.nih.gov/books/NBK7637/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1518391/
https://www.cdc.gov/pneumonia/atypical/mycoplasma/index.html
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5689399/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3565243/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6388746/pdf/ijgm-12-101.pdf
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6388746/
https://pubmed.ncbi.nlm.nih.gov/23400696/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2413218/