What are Some Root Causes For Fibromyalgia?
Fibromyalgia affects millions of people throughout the world and conventional medicine has yet to discover meaningful solutions to this rapidly spreading condition. However, in recent years there has been an increase in research on the underlying causes associated with fibromyalgia, a condition that causes pain in soft tissues and muscles throughout the body. Other symptoms associated with fibromyalgia include:
Joint Pain
Headaches / Migraines
Gastrointestinal Issues (IBS, Food Sensitivities, Painful Bloating, Gluten Intolerance)
Burning and/or Twitching Muscles
Multiple Chemical Sensitivity (MCS)
Essentially, fibromyalgia is a cluster of symptoms that is labeled as a condition. Fibromyalgia can be a symptom of a larger underlying problem and is diagnosed when a doctor cannot pinpoint the root cause. Since there are no known tests to test for this condition, conventional doctors typically rely on a patient’s list of symptoms. Later, they may be prescribed a prescription medication to inhibit inflammation and reduce pain. However, this approach is not often reliable as it can suppress symptoms yet continues to look over the root causes of the condition.
What are the Root Causes of Fibromyalgia?
1) Gut Infections: Gastrointestinal issues and an altered gut microbiome are common amongst Fibromyalgia patients. Since the majority of the body’s intelligence symptom is located within the gut, a dysfunctional gastrointestinal tract may often cause pain and discomfort to radiate from the gut to other extremities in the body, creating symptoms of fibromyalgia, arthritis, and other pain disorders.
When the gut’s beneficial bacteria is overthrown by pathogenic bacteria, it may lead to an array of so-called “unexplained” symptoms. People struggling with fibromyalgia may have gut issues such as:
h. Pylori Infection: h. Pylori is a gram-negative bacteria that infects the stomach and is known to cause long term intestinal permeability, food sensitivities, abdominal pain, constipation, etc. A 2011 study states that a “former h. Pylori infection may have a role in the etiopathogenesis of fibromyalgia syndrome or may act as a triggering factor.”
A 2020 study stated that their experimental fibromyalgia group “reported a significant reduction in pain, as evaluated by the number of tender points, following H. pylori eradication.”
2) Unbalanced Firmicutes to Bacteroidetes Ratio: Firmicutes and Bacteroidetes are types of bacteria that account for 90% of the gut microbiota. They assist in carbohydrate metabolism, energy production and conversion, amino acid transport, metabolism, and production of short-chain fatty acids (SCFAs). A balanced ratio between these two types of bacteria is crucial for a healthy gut. When unbalanced, the body may experience obesity and Inflammatory Bowel Disease (IBD/IBS).
A 2019 study found that an imbalance of “Bacteroides genera, including Bacteroides dorei, Bacteroides uniformis, Bacteroides stercoris, Bacteroides ovatus, as well as Prevotella copri, Alistipes putredinis, and Faecalibacterium prausnitzii” were abundantly found amongst fibromyalgia patients.
Additionally, another 2019 study stated that overall “the diversity of bacteria is reduced in fibromyalgia patients.”
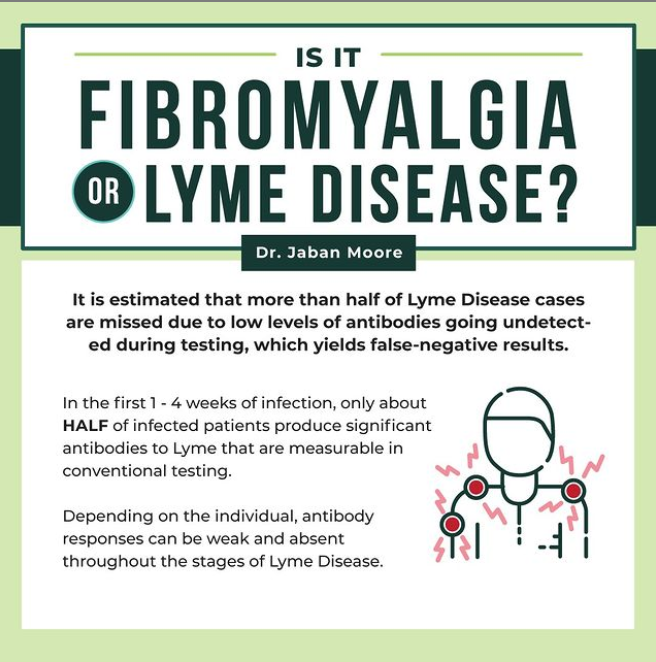
3) Bacterial Infections: Generally, any gut infection can cause symptoms of chronic fatigue, gastrointestinal issues, muscle/joint pain, and mental disorders which may form into fibromyalgia. An overlooked bacterial infection that causes fibromyalgia is Lyme Disease and its co-infections. Small Intestinal Bacterial Overgrowth (SIBO) and candida are possible root causes as well.
Click here to read our article on Lyme Disease!
4) Parasites: Like bacterial infections, parasites cause damage in the gastrointestinal tract, brain, joints, muscles, etc., making it easy for symptoms of fibromyalgia to show. Oftentimes, parasites cause nutritional deficiencies, making experiencing symptoms of fibromyalgia at a higher risk.
Click here to read our article on parasitic infections and chronic illnesses!
5) Toxicities: As humans, we are chronically exposed to toxins such as: food additives, environmental pollution, cleaning chemicals, heavy metals, mold, and water contaminants. Constant exposure to these toxins may result in chemical sensitivities, mold illness (CIRS), and inflammatory symptoms that appear as fibromyalgia.
A 2021 study stated that “heavy metals such as aluminium induce oxidative stress parameters and decrease the levels of essential trace elements such as magnesium and zinc, which may be responsible for the severity of fibromyalgia.”
A 2013 study stated that exposure to mold and mycotoxins was present in “90%” of chronic fatigue syndrome patients. These patients also experienced fibromyalgia. According to this study “additional symptoms in chronic fatigue syndrome patients include fibromyalgia, headaches, loss of balance, neurocognitive difficulties, flu-like symptoms, irritable bowel syndrome, anxiety, depression, among others symptoms.” These symptoms overlap with fibromyalgia and are closely related.
6) Nutrient Deficiencies: If an individual is not receiving enough nutrients or absorbing enough nutrients, problems may arise. Nutrient deficiencies commonly seen in fibromyalgia patients include:
Magnesium: A 2021 study stated that “magnesium deficiency has been largely associated with muscle pain along with fatigue, sleep difficulties, and anxiety; all of which are common symptoms of fibromyalgia. In some studies, it is thought that magnesium deficiency, through reductions in muscle ATP levels, may play a role in the development of fibromyalgia. Other studies correlate increased levels of substance P (a neurotransmitter known for its role in pain perception) with magnesium deficiency as well as pain intensity in fibromyalgia.”
Vitamin D: A 2011 study stated that “vitamin D deficiency has to be considered in the management of fibromyalgia syndrome.” Low levels of this vitamin may alter hormones and the gut microbiome.
Glutathione: A 2009 study stated that “glutathione and catalase levels were significantly lower in fibromyalgia patients than controls… Additionally, the correlation between glutathione level and morning stiffness was found to be significant.” Glutathione is the body’s main detoxifying antioxidant. When it is found in low levels, the body may struggle to detox unwanted substances and toxicities.
Selenium: A 2018 study stated that “Muscle pain has been associated with deficiencies in amino acids, magnesium, selenium, vitamins B and D, as well as with the harmful effects of heavy metals, such as mercury, cadmium, and lead. Research indicates that patients deficient in certain essential nutrients may develop dysfunction of pain inhibitory mechanisms together with fatigue and other fibromyalgia symptoms. Additionally, mercury and other toxic elements may interfere with the bioavailability of essential nutrients.”
6) Injury / Physical & Emotional Trauma: Injury and physical/emotional trauma may cause chronic inflammation which can lead to fibromyalgia symptoms. Chiropractic care, therapy, acupuncture, and other healing modalities may be used.
Click here to read our article on trauma and chronic illnesses!
If you believe you are dealing with chronic illness, please contact a functional provider. Dr. Jaban Moore, a functional medicine provider, can help you if you are experiencing chronic symptoms.
Please reach out if you are interested in taking your health back! You can give our office a call at (816) 889-9801.
References:
https://www.sciencedirect.com/science/article/abs/pii/S0025619611652233
https://arthritis-research.biomedcentral.com/articles/10.1186/ar4395
https://link.springer.com/article/10.1186/s12955-014-0111-6
https://www.sciencedirect.com/science/article/abs/pii/0002934393900854
https://headachejournal.onlinelibrary.wiley.com/doi/abs/10.1111/head.12590
https://link.springer.com/article/10.1007/s11916-996-0009-z
https://ctajournal.biomedcentral.com/articles/10.1186/2045-7022-3-S3-P120
https://pubmed.ncbi.nlm.nih.gov/16331775/
https://www.tandfonline.com/doi/abs/10.1080/08869634.2019.1650215
https://europepmc.org/article/med/1466872
https://www.sciencedirect.com/science/article/abs/pii/S1524904215000806
https://www.liebertpub.com/doi/abs/10.1089/jwh.2006.15.1035
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7285218/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6351938/
https://www.sciencedirect.com/science/article/pii/S0255085720302668
https://pubmed.ncbi.nlm.nih.gov/31327695/
https://link.springer.com/article/10.1186/1743-7075-7-79
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4863046/
https://www.hoffmancentre.com/wp-content/uploads/pdfs/am/Chronic_Inflammatory_Response_Syndrome.pdf
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3705282/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3705282/
https://journals.sagepub.com/doi/full/10.1177/21501327211038433
https://pubmed.ncbi.nlm.nih.gov/21894355/
https://pubmed.ncbi.nlm.nih.gov/18853166/
https://www.sciencedirect.com/science/article/abs/pii/S0753332218309697