Ehrlichia - A Sneaky Lyme Co Infection
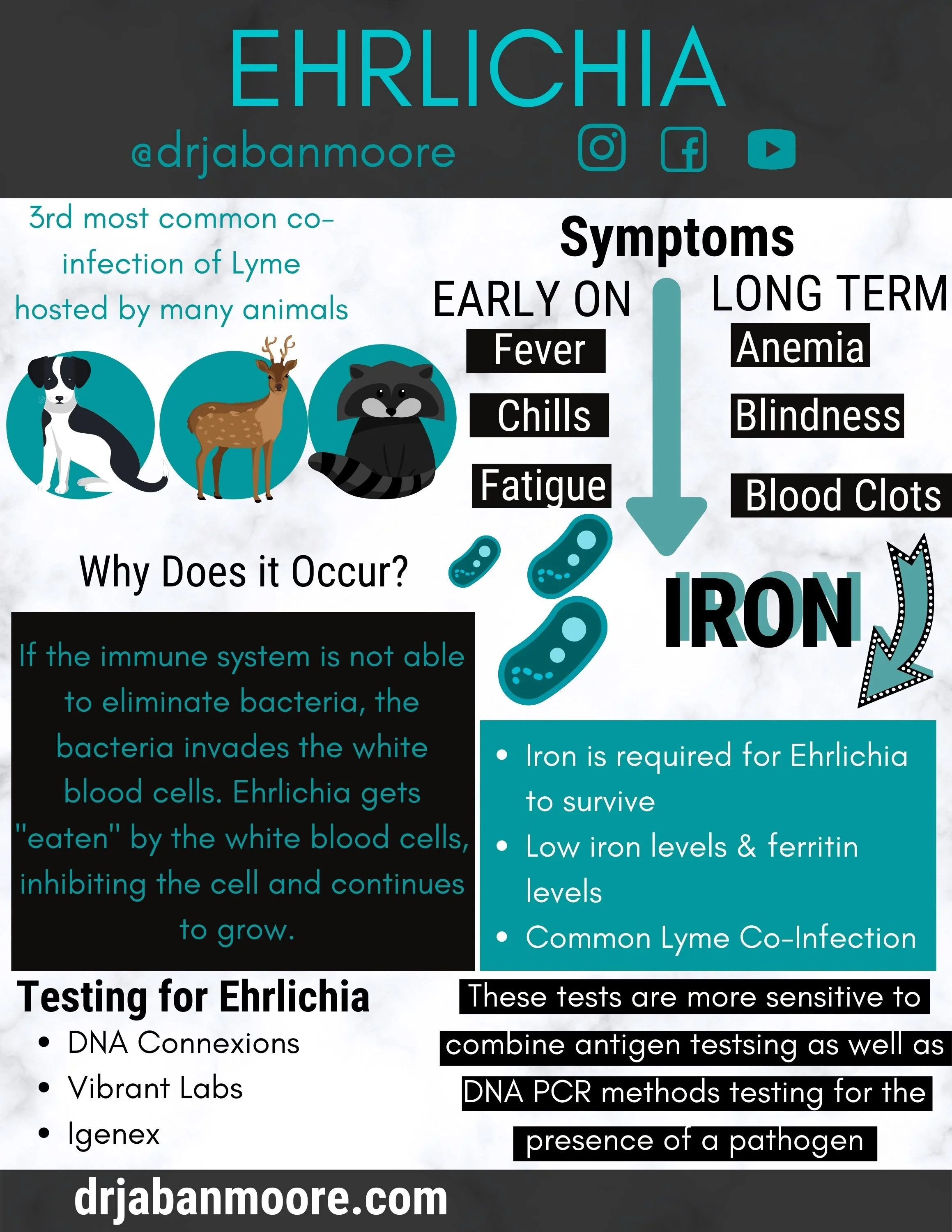
Ehrlichia, the third most common co-infection found with Lyme, is a bacteria that invades and lives inside of white blood cells. Hosts can vary, all the way from humans and pets, like dogs and goats, to wild animals, especially white-tailed deer, coyotes, and racoons. There is currently more information on Ehrlichia in the veterinary world than in human medicine. Veterinarians confirm that ehrlichiosis can be a chronic condition, while human medicine does not acknowledge this and says the infection is only acute!
First identified in 1987, Ehrlichia is most commonly found in the eastern half of New England to western Texas. In a meta-study done from 1986-1997, there were 145 cases identified in Missouri, 55 in Georgia, 53 in Texas and 52 in Arkansas. Currently, there are over 1,700 cases of Ehrlichiosis diagnosed per year, 35% of which come from Arkansas, Oklahoma, and Missouri, most likely due to high populations of white-tailed deer within these areas (1).
Types of Ehrlichia
There are several types of Ehrlichia that inhabit different white blood cells. Human Monocytic ehrlichiosis is caused by Ehrlichia Chaffeensis, which is transmitted by the lone star tick. Due to this, symptoms can vary when present.
Early signs within the first week include:
Fever
Chills
Fatigue
Low back pain
Muscle aches
Gastrointestinal symptoms like vomiting and/or diarrhea
Swollen lymph nodes
Longer term symptoms can be more severe, including:
Anemia
Eye problems - like blindness and recurrent pink eye
Painful or difficult urination
Neurological issues
Swollen limbs
Bleeding episodes from the inability of blood to clot due to low platelets and/or low blood pressure.
In more severe cases, Ehrlichia can damage lungs, liver, spleen, kidneys, blood vessels, lymph nodes, and the nervous system causing kidney failure, liver failure, and/or adrenal insufficiency. A rash can also form on extremities, trunk, or face in later course of infection, but it does not necessarily appear at the site of a bite like the bullseye rash commonly associated with Lyme Disease. Only 20% of people infected will develop symptoms of nervous system damage including facial palsy, tremors and twitches, cognitive impairment, photophobia (light sensitivity), seizures, confusion, and/or problems with cranial nerves (which can impair many things such as smell or taste), while 20-25% experience severe respiratory problems (1). People infected typically present as asymptomatic or with mild symptoms, however, for the elderly or immunocompromised, it can be fatal.
Why does Ehrlichia Occur?
Ehrlichiosis occurs if the immune system is not able to eliminate bacteria before it invades white blood cells. Ehrlichia has evolved complex mechanisms to evade the immune system. White blood cells are usually highly effective at killing pathogens by phagocytizing (or eating) them and destroying them. Ehrlichia gets eaten, but not destroyed, and inhibits the white blood cell from apoptosis (programmed cell death) allowing it to continue growing and living (2). In one study, healthy mice that were infected with Ehrlichia and the infection was cleared within 16 days (1). In immunocompromised mice, the infection was present for months. This concept is similar in humans. In another study in Tennessee, golfers with poorer scores were more likely to have antibodies reactive with E. chaffeensis, presumably because their lack of skill placed them more frequently in the wooded or grassy locations adjacent to the fairway, where ticks abound. Additionally, military personnel participating in field exercises in New Jersey and Arkansas were more likely to carry these same reactive antibodies. E. chaffeensis was actually first isolated in Fort Chaffee Arkansas, where the bacteria got its name (1)!
Diagnosing Ehrlichia
Ehrlichia is not a new disease, as it has been around for a long time, but it is becoming more and more of a problem as we become a sicker population. So how is it diagnosed? Ehrlichia needs iron to survive (1), making it a contributor to low iron levels, anemias, and/or high ferritin levels, possibly to hide iron from the feeding pathogen. Clinically, one would see low transferrin with Ehrlichia as well. It is also a common Lyme co-infection that is likely transmitted at same time via tick bite, thus causing immunosuppression, so many times, you will also see the presence of Candida and Aspergillus.
Routine laboratory results indicative of an infection include a low white blood cell count, and low platelet count, as well as elevated liver enzymes (ALT, AST, LDH), elevations in the levels of serum creatinine and amylase, and electrolyte abnormalities including low serum sodium, magnesium, calcium, and phosphorus. A confirmed diagnosis can be made using an antibody IFA (Immuno-Fluorescent Assay). In severe cases, blood smears can be examined for ehrlichiosis and is most effective during the first week after infection (3). Like other stealth pathogens, a confirmed diagnosis can be difficult to obtain. The lab tests I run the most often include DNA Connexions, Vibrant Labs or Igenex as the tests are more sensitive when they combine antigen testing as well as DNA PCR methods to test for the presence of a pathogen.
Once a diagnosis is confirmed, conventional treatment consists of antibiotics like doxycycline, cipro, gentamicin, penicillin, and/or erythromycin. Western doctors often do not even wait for lab results to come back and immediately begin antibiotics if symptoms are present. For a more natural approach, a treatment plan would consist of support for the white blood cells, medicinal mushrooms, and the use of killer herbs.
(1) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC145301/
(2) https://europepmc.org/article/med/16406779
(3) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2882064/